Abstract
Background: Human parvovirus B19, a common childhood infection that typically causes mild disease in healthy individuals, causes life-threatening anemia due to transient red cell aplasia (aplastic crisis) in individuals with sickle cell disease (SCD). This complication often leads to hospitalization and red blood cell transfusions. Limiting the amount of transfusions is imperative to avoid alloimmunization. Strategies to mitigate complications from parvovirus B19 or reduce disease severity in SCD patients are needed. In this prospective observational study, we aim to describe the relationship between vitamin A and D levels and severity of symptoms during parvovirus B19 infection in pediatric patients with SCD.
Methods: Twenty pediatric patients with SCD admitted to St. Jude Children's Research Hospital experiencing aplastic crisis and identified as having an active parvovirus B19 infection were under an IRB approved protocol (NCT02261480) and followed prospectively for 120 days post-infection. Acute parvovirus B19 infection was diagnosed by fever and a positive virus-specific IgM ELISA or PCR. Aplastic crisis was defined by worsened anemia without sufficient compensatory reticulocytosis in the setting of an acute parvovirus B19 infection. Virus-specific antibody responses were measured from sera or nasal washes (NW) by ELISA using parvovirus B19 virus-like particles (VLP) as target antigens. Peak serum antibody titers were defined (among measurements from Days 0, 7, 30, and 120). Total erythrocyte transfusion volumes required during the admission were quantified. Hematologic indices and vitamin A and D levels were obtained on Day 0. Vitamin A (retinol) was measured using UPLC and vitamin D (25[OH]D) was measured using a Roche Elecsys Vitamin D ELISA. Statistical analyses were performed with Spearman's rank correlation coefficient or Mann Whitney tests. We scored significance as p<0.05.
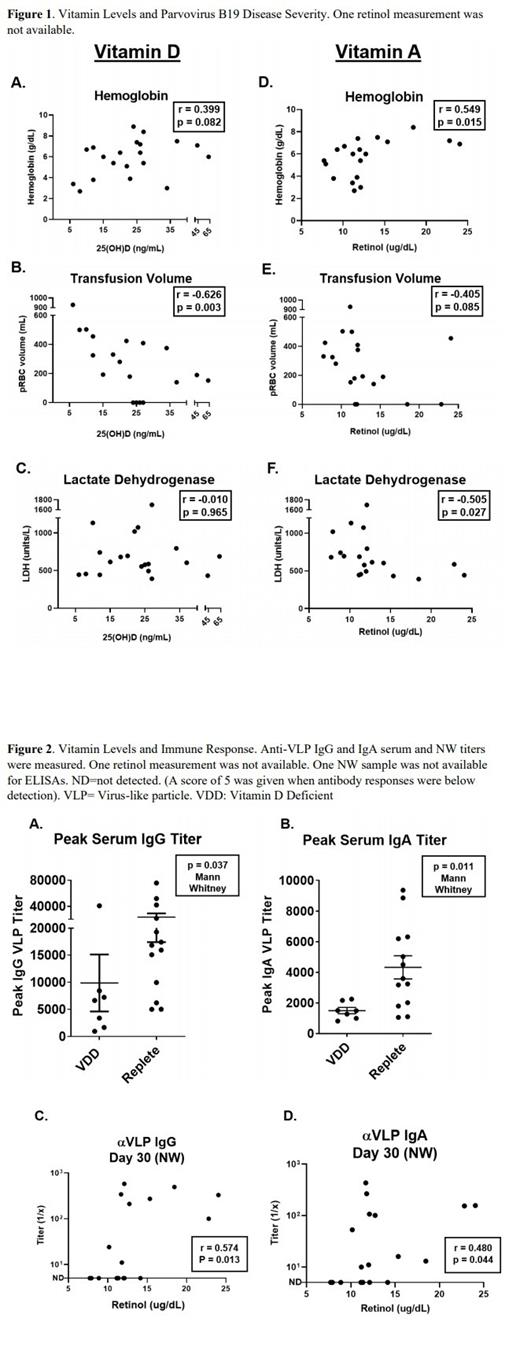
Results: Twenty patients with different genotypes of SCD requiring hospital admission due to acute parvovirus B19 infection were sequentially enrolled (15 HbSS, 3 HbSC, 1 HbSD, 1 HbSβeta +thalassemia). Thirty-five percent (7/20) of patients were vitamin D deficient (VDD, defined here as <20 ng/mL) while 89% (17/19, one sample was not measured) of patients were marginally or severely vitamin A deficient (defined here as <20 μg/dL) on Day 0. Correlative analyses between vitamin levels and markers of disease severity are shown in figure 1. Lower vitamin D levels trended with lower hemoglobin (r=0.399, p=0.082) and there was a significant inverse correlation between transfused volume and vitamin D levels (r=-0.626, p=0.003, Figure 1B). There was a significant positive correlation of vitamin A levels on Day 0 with hemoglobin concentration (r=0.549, p=0.015, Figure 1D), and an inverse correlation between vitamin A levels and lactate dehydrogenase (r=-0.505, p=0.027, Figure 1F).
Children with replete vitamin D levels exhibited significantly better peak virus-specific serum IgG (p=0.037) and IgA (p=0.011) responses (Figure 2A-B). Additionally, vitamin A, which plays an important role in mucosal immunity, correlated positively with virus-specific IgG (r=0.574, p=0.013) and IgA (r=0.480, p=0.044) in nasal passages on Day 30 (Figure 2C-D).
Conclusions: In pediatric patients admitted to the hospital for acute parvovirus B19 infection, low vitamin A and D levels were associated with greater disease severity (greater hemolysis, lower hemoglobin concentration, and greater transfusion volumes). Higher vitamin levels were associated with better virus-specific antibody responses. While cause-effect relationships were not discerned in this study, we hypothesize that poor nutritional status contributed to poor outcomes and that efforts to improve nutrition may reduce the severity of parvovirus B19 disease in patients with SCD.
Hankins: UpToDate: Consultancy; Vindico Medical Education: Consultancy; Global Blood Therapeutics: Consultancy; Bluebird Bio: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal